- History & Evolution
- Biosynthesis vs. dietary uptake
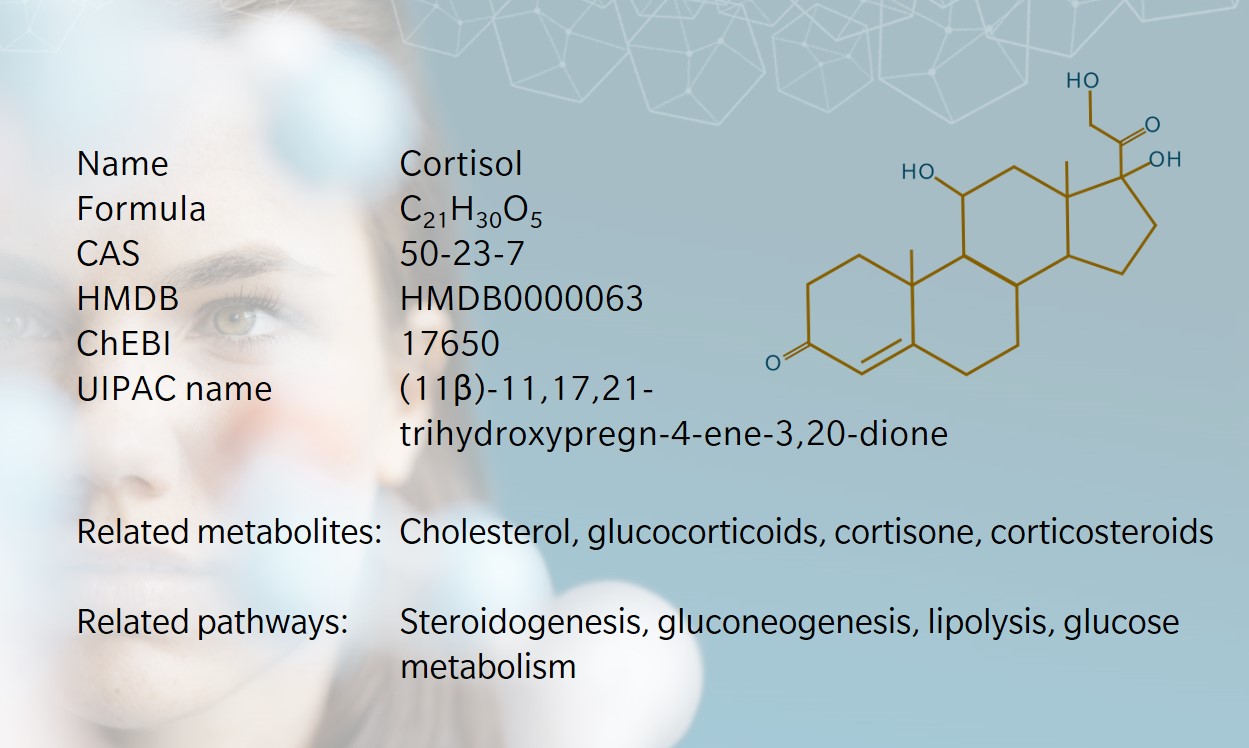
- Cortisol – a versatile steroid hormone
- Cortisol and stress
- Cortisol, obesity, and diabetes
- Cortisol and the immune system
- Cortisol and other organs
History and evolution
1937: first isolation (Ghaddhab et al. 2017) | 1946: first synthesis ( (Timmermans et al. 2019) | 1950: anti-inflammatory role first identified
Cortisol’s story begins in the mid 19th century, when British physicist Thomas Addison established the role of the adrenal cortex and first described symptoms of adrenal deficiency, now known as Addison’s disease (Timmermans et al. 2019). In 1937, Tadeus Reichstein isolated cortisol from the adrenal glands. A decade later, rheumatologist Philip Hench showed that cortisol, and specifically its derivative cortisone, could be used to treat rheumatoid arthritis and other inflammatory conditions. Reichstein and Hench (and fellow researcher Edward Kendall) were jointly awarded a Nobel Prize in 1950 for their discoveries.
Cortisol is a glucocorticoid steroid hormone, released by the adrenal glands in response to biochemical stress. Cortisol gets bad press as the body’s “stress hormone”, but without an effective stress response the organism’s survival would be in jeopardy. Cortisol also kicks into gear when other physiological responses go awry, helping to maintain homeostasis.
Biosynthesis vs. dietary uptake
Cortisol is synthesized from cholesterol and secreted from the zona fasciculate of the adrenal cortex (Lee et al. 2015). This follows a complex chain of hormonal reactions and interactions, which starts in the brain. The hypothalamus secretes corticotropin-releasing hormone (CRH), which causes cells in the anterior pituitary to release adrenocorticotropin hormone (ACTH) into the vascular system. ACTH is transported to the adrenal cortex via the blood, where it increases low density lipoprotein receptors and cholesterol desmolase. Cholesterol is converted to pregnenolone, which is the precursor for cortisol and other glucocorticoids. The reaction is catalyzed by the hydroxylase enzyme CYP17A1. Further enzymatic reactions complete the conversion to cortisol.
CRH can be released in response to stress, intensive exercise, low blood glucose levels, and viral infections. Increased cortisol levels suppress the release of CRH and ACTH in a negative feedback loop that keeps all three in check (Winter et al. 2012). The hypothalamus-pituitary-adrenal (HPA) axis follows a circadian rhythm, giving cortisol a diurnal cycle with higher levels in the morning and lower levels in the evening (Thau et al. 2021).
The main downstream product of reversible cortisol metabolism is cortisone. This occurs via the 11-beta hydroxysteroid dehydrogenase system (11-beta HSD1 and 11-beta HSD2) (Tomlinson et al. 2004). Any cortisol and cortisone products that aren’t needed are broken down into tetrahydrometabolites in the liver, before being flushed out in urine (Stachowicz et al. 2016).
Cortisol – a versatile steroid hormone
Cortisol helps regulate multiple physiological functions, including inflammatory response, metabolism and immune function (Thau et al. 2021), but it’s best known for mediating the body’s reaction to stress.
Exposure to stress triggers the “fight or flight” response, which begins in the amygdala. If the amygdala determines the threat level to be serious enough, it signals to the hypothalamus to activate the sympathetic nervous system. This prompts the adrenal glands to release a surge of epinephrine and cortisol. While one wouldn’t want to remain in this state for long, cortisol allows the body to remain on high alert and prepare to fend off danger, ensuring a quick release of energy to the parts of the body that need it (Thau et al. 2021).
Beyond the stress response, cortisol also aids glucose metabolism, stimulating gluconeogenesis and making energy available to the brain, liver, muscles, adipose tissue, and pancreas.
In adipose tissue, cortisol increases lipolysis, releasing free fatty acids which provide energy to other cells. In the pancreas, cortisol decreases insulin levels and increases glucagon, which in turn promotes glycogenolysis, gluconeogenesis, and ketogenesis in the liver (Thau et al. 2021). In the brain, cortisol can affect appetite, mood, and pain perception. And cortisol supports the immune system by slowing the migration of white blood cells to inflamed sites and stimulating the body’s response to injury (Stachowicz et al. 2016).
Cortisol and stress
Cortisol has been broadly accepted as a reliable biomarker of stress. According to the glucocorticoid cascade hypothesis, chronic exposure to stress causes consistently elevated cortisol levels, which do not return to baseline even when the source of stress abates (Lee et al. 2015).
Persistently elevated cortisol concentrations are associated with metabolic disorders including raised blood pressure, insulin resistance, bone abnormalities, and calcium deficiency (Stachowicz et al. 2016).
Given the complex relationship between sociological and physiological causes and effects of stress, Roberts and McWade call for a new “cortisol sociology”, encouraging sociologists to engage with cortisol research to build a better understanding of the overlap and distinction between biological and social factors in stress-related disease (Roberts et al. 2021).
Cortisol, obesity, and diabetes
As with many metabolites, the dose makes the poison. For example, in diabetic patients with hypoglycemia, the right amount of cortisol can help bring blood sugar levels back to normal levels. On the other hand, cortisol is known to have diabetogenic effects, by inhibiting insulin secretion and signaling (Dallman et al. 1993).
A 2020 study found that cortisol is associated with higher blood glucose levels in people with type 2 diabetes (Dias et al. 2020). Cortisol’s diurnal cycle was also found to be less pronounced in people with higher glucose levels. In this study, body mass index did not appear to affect the results. However, other research has found that individuals with obesity may be less able to compensate for the long-term effects of cortisol and stress on insulin resistance, leading to hyperglycemia (Al-Goblan et al. 2014, Adam et al. 2010).
Cortisol’s relationship with weight gain is complicated. Some people may overeat in response to stress, while others may lose their appetite. Studies show that CRH is released following a stressful event, which suppresses the need to find food so that the individual can focus on addressing the threat (Sominsky et al. 2014). Once the threat has passed, the desire to eat and replace spent energy returns. Chronic stress interferes with the HPA axis to disrupt appetite and eating behavior. In this way, cortisol is linked to obesity, which brings a higher risk of metabolic syndrome, heart disease, and diabetes.
Cortisol and the immune system
Cortisol has been shown to reduce inflammation signaling, leading to the use of cortisone and other corticosteroids to treat inflammation in rheumatoid arthritis, osteoporosis, sciatica, and chronic joint and muscular pain.
Conversely, dysregulated cortisol can result in inflammation, which links chronic stress with several inflammatory autoimmune diseases (Hannibal 2014). Persistent and widespread inflammation can affect the immune system and trigger the growth of cancerous cells (Morrison 2012).
An effective immune response relies on T cell homeostasis, particularly the ratio of T-helper 1 (Th1) and T-helper 2 (Th2) cytokines. Th1 cells promote cellular immunity, while Th2 cells promote humoral immunity. Cortisol is thought to trigger a shift from Th1 to Th2 cells, which then changes the dominant immune response, with implications for different disease types (Elenkov 2004).
Cortisol and other organs
In the brain, cortisol has effects on memory, mood, and neurological diseases. Chronic high cortisol has been shown to impair learning and reduce brain function in older people (Sroykham et al. 2019). Elevated cortisol levels and a flattened diurnal cortisol curve are associated with depression (Stetler et al. 2011).
In the kidneys, cortisol is essential for healthy blood flow and glomerular filtration rate – but again, the amount is important. Elevated plasma cortisol is found in patients with chronic kidney disease (CKD). Assessing cortisol metabolism is challenging in patients with CKD because of the kidney’s role in cortisol excretion. CKD can mask symptoms of excess cortisol in patients with Cushing’s disease (Stroud et al. 2019).
Elevated cortisol levels are also associated with changes in bone homeostasis (Raff et al 1999). Acute stress can trigger adaptive skeletal remodeling, but prolonged stress can cause bone mineral loss. Cushing’s disease is also linked to osteoporosis and bone fractures (Ng et al. 2021).
References
Adam T. et al: Cortisol Is Negatively Associated with Insulin Sensitivity in Overweight Latino Youth. (2010) Journal of Clinical Endocrinology & Metabolism | https://doi.org/10.1210/jc.2010-0322
Al-Goblan A. et al.: Mechanism linking diabetes mellitus and obesity. (2014) Diabetes, Metabolic Syndrome and Obesity | https://doi.org/10.2147/DMSO.S67400
Dallman M. et al.: Feast and Famine: Critical Role of Glucocorticoids with Insulin in Daily Energy Flow.” (1993) Frontiers in Neuroendocrinology | https://doi.org/10.1006/frne.1993.1010
Dias J. et al.: The longitudinal association of changes in diurnal cortisol features with fasting glucose: MESA. (2020) Psychoneuroendocrinology | https://doi.org/10.1016/j.psyneuen.2020.104698
Elenkov I.: Glucocorticoids and the Th1/Th2 balance. (2004) Annals of the New York Acadamy of Science | https://doi.org/10.1196/annals.1321.010
Ghaddhab C. et al.: From Bioinactive ACTH to ACTH Antagonist: The Clinical Perspective (2017) Frontiers in Edocrinology | https://doi.org/10.3389/fendo.2017.00017
Hannibal K. et al.: Chronic Stress, Cortisol Dysfunction, and Pain: A Psychoneuroendocrine Rationale for Stress Management in Pain Rehabilitation. (2014) Physical Theraphy & Rehabilitation Journal | https://doi.org/10.2522/ptj.20130597
Lee D. et al.: Technical and clinical aspects of cortisol as a biochemical marker of chronic stress. (2015) BMB Reports | http://doi.org/10.5483/BMBRep.2015.48.4.275
Morrison W.: Inflammation and cancer: a comparative view.” (2012) Journal of Veterinary Internal Medicine | https://doi.org/10.1111/j.1939-1676.2011.00836.x
Ng J. et al.: Potential mechanisms linking psychological stress to bone health. (2021) Internal Journal of Medicine and Science | https://doi.org/10.7150/ijms.50680
Raff H. et al.: Elevated salivary cortisol in the evening in healthy elderly men and women: correlation with bone mineral density. (1999) The Journals of Gerontology | https://doi.org/10.1093/gerona/54.9.m479
Roberts C. et al.: Messengers of stress: Towards a cortisol sociology.. (2021) Sociology of Health and Illness | https://doi.org/10.1111/1467-9566.13261
Sominsky S. et al.: Eating behavior and stress: a pathway to obesity. (2014) Frontiers in Psychology | https://doi.org/10.3389/fpsyg.2014.00434
Sroykham W. et al.: Effects of brain activity, morning salivary cortisol, and emotion regulation on cognitive impairment in elderly people. (2019) Medicine | https://doi.org/10.1097/MD.0000000000016114
Stachowicz M. et al.: The effect of diet components on the level of cortisol. (2016) European Food Research and Technology | https://doi.org/10.1007/s00217-016-2772-3
Stetler C. et al.: Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. (2011) Psychosomatic Medicine | https://doi.org/10.1097/PSY.0b013e31820ad12b
Stroud A. et al.: Diagnosing Cushing’s disease in the context of chronic kidney disease: a case report and literature review. (2019) European Journal of Endocrinology | https://doi.org/10.1530/ EJE-19-0326
Thau L. et al.: Physiology, Cortisol. (2021) StatPearls | https://pubmed.ncbi.nlm.nih.gov/30855827/
Timmermans S. et al.: A General Introduction to Glucocorticoid Biology. (2019) Frontiers in Immunology | https://doi.org/10.3389/fimmu.2019.01545
Tomlinson J. et al.: 11β-Hydroxysteroid Dehydrogenase Type 1: A Tissue-Specific Regulator of Glucocorticoid Response. (2004) Endocrine Reviews | https://doi.org/10.1210/er.2003-0031
Winter, W. et al.: Cortisol: Clinical Indications and Laboratory Testing. (2012) Clinical laboratory news | https://www.aacc.org/cln/articles/2012/september/cortisol